Joint Replacement Guide
We develop orthopedic implants with patients and physicians in mind.

We believe that movement is joy and enables us to connect with others. That is why we are committed to restore the eMotion of Motion through orthopedics.

We know that debilitating joint conditions and pain can interfere with every aspect of your life. Pain can prevent walking, exercising, working, enjoying time with family and friends, or even getting a full night’s sleep. Whilst joint replacement procedures are routine, it is still important that you prepare ahead of surgery.


It is important you feel completely comfortable and understand the process and your recovery. To help, we have prepared a list of FAQs here.
Our Products

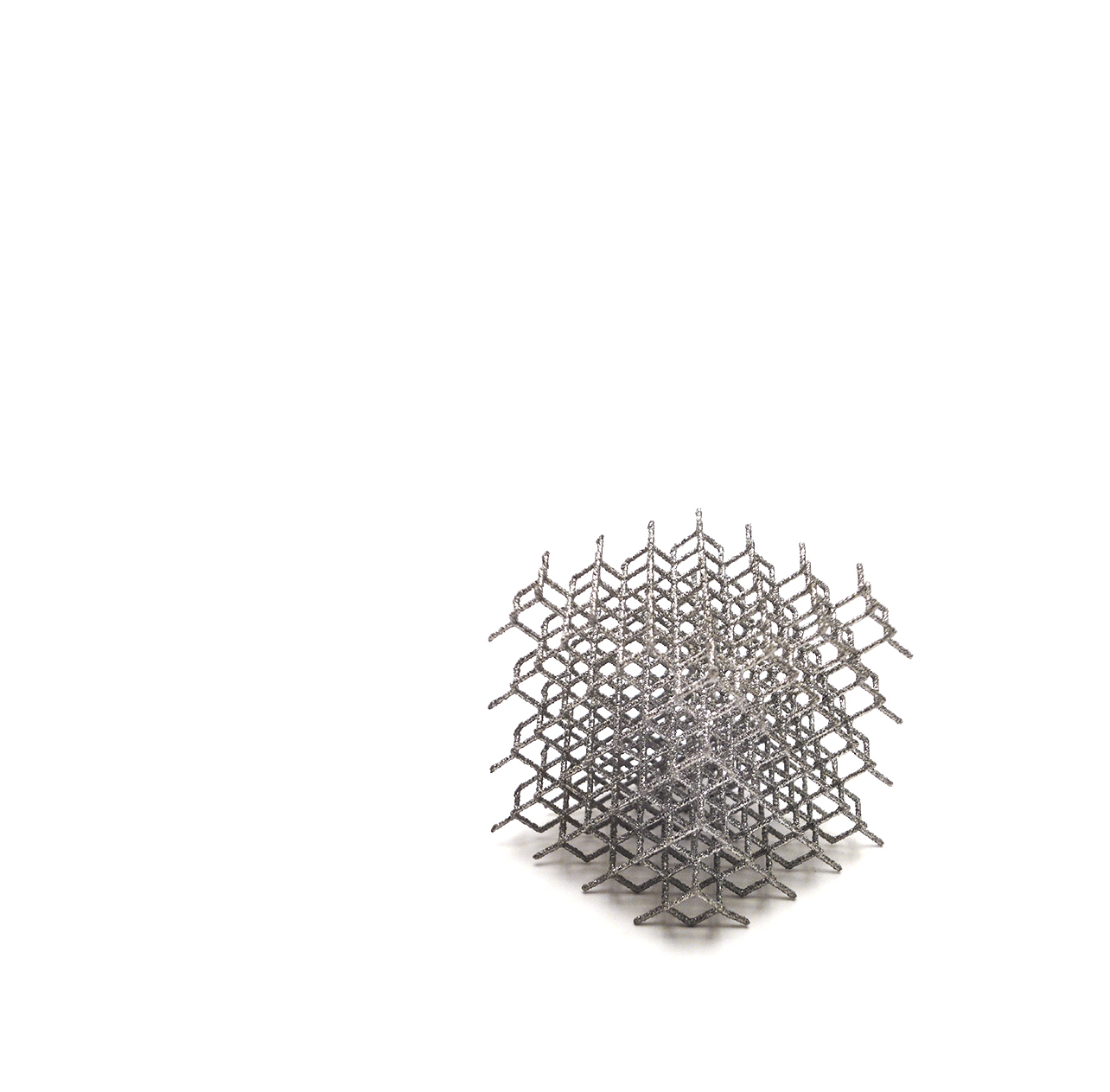
Most LimaCorporate products are created using Titanium, a material used in most orthopedic implants. Our heritage of working with Titanium dates to 1970. In 2007 we patented Trabecular Titanium (TT), a new 3D printed technology that better supports new bone formation.
It is often chosen by physicians for treating severe articular diseases and deformities. This surgeon, for instance, used ProMade to restore her patient's motion after a car crash.

Joint Disease
Joint Replacement
Surgery

Before you have joint replacement surgery, consider the following steps and discuss them with your orthopedic surgeon.
Pre-surgery tests and visitsPatients are required to share routine blood and urine samples for analysis at least 14 days (two weeks) before surgery. You should also undergo a physical examination within 30 days (one month) of your surgery date. Patients over 50 and/or with a history of cardiac or respiratory issues should also have an EKG and chest x-ray during this time. The majority of pre-admission testing will be conducted by your personal physician or hospital.
MedicationBefore orthopedic surgery, you must verify with your surgeon if your usual medication(s) are compatible with the procedure. If not, the orthopedic physician may ask you to stop or change medication.
Immediately before your surgery, the anaesthesiologist will give you an injection to help you relax. It's normal for your mouth to feel a little dry.
Operating RoomYou will discuss the anaesthetic that suits your orthopedic surgery best with your anaesthetist. Anaesthetic can be administered either as ‘general’ or ‘spinal’. ‘Spinal’ is only given to patients undergoing knee and hip operations as it numbs the legs/lower torso without putting a patient fully to sleep.
Next, you will stay in the pre-surgery area where healthcare professionals may place an intravenous (IV) drip in your veins. This drip helps you receive fluids and medications during your surgery.
When everything is ready, the hospital staff will take you to the operating room and will help you onto the operating table. They may measure your blood pressure and place an oxygen mask over your mouth and nose, so you are comfortable breathing.
If you are given a ‘general’ anaesthetic, you will fall asleep shortly afterwards. You won’t feel any pain and won't be aware of anything that happens during surgery. If you are given ‘spinal’ anaesthetic or for a specific body part/area, the joint area will become totally numb, and you won’t feel any pain. You may also receive extra medicine from the anaesthetist that helps you to drift in and out of sleep.
Waiting AreaYour family and friends will be told where to wait while you are in the operating room. After surgery, your orthopedic surgeon will talk to your family and update them on your recovery. Visitors are normally permitted once surgery is complete, and patients have spent sufficient time in recovery.

Your surgeon begins by cutting the skin so that nerves and blood vessels can be isolated and moved aside. Any muscles in the area are also moved to give a complete view of the joint. The surgeon can now replace the damaged body part(s) with the orthopedic implant(s).
Once an implant has been inserted and fits, the physician will close the incision with multiple layers of stitches or metal staples. The incision will be dressed in a bandage and the patient is returned to the recovery room.

When you first wake up you will most likely feel ‘groggy.’ This feeling is caused by the medications and anaesthetic you received during surgery. Once your surgeon is happy with your recovery, the medical staff will take you to your room.
When you are fully awake, you will be able to eat and drink – take this slowly and only what you feel you can manage at the time. Nurses will continue to check your vital signs, urinary output, and any drainage.
Make sure to talk with your doctor before surgery about your pain management options. You may receive pain relief through your IV drip, through an epidural, shots, or in pill form. Medicine(s) may also be administered intravenously by a ‘pain pump’ for the first 24 hours. This allows medical staff to control your pain medication up to a predetermined dosage. The healthcare team will also help you adapt your daily activities to your ability post-surgery.

After your surgery, your orthopedic surgeon, nurses, and therapists will monitor your condition and track your progress. Most patients stay in hospital for between one to four days following their surgery. However, this depends on many factors and your surgeon will decide the best option for you.
Whatever the joint, you'll need to exercise to aid its recovery and rehabilitation. Your recovery plan may even start on the very same day of your surgery. Your Physical Therapist will give you specific exercises to perform at home, designed to increase your range of motion, mobility, and strength. They will also recommend safe activities for you and will review your exercise program throughout your weeks of recovery.
Once home, at first you will need help with basic tasks, including housework, driving, shopping, and preparing meals. You can expect to regain your strength and endurance as you begin to take on more of your normal daily routine.
Any post-surgery pain should be temporary. Most patients with artificial joints are able to enjoy many of their ‘old’ activities once again. However, high impact exercises may damage a new joint and cause it to wear down again. You should choose low-impact activities such as swimming and walking, and it is important you verify with your orthopedic surgeon what you can or cannot do.
Limacorporate S.p.A., as a manufacturer of prosthetic implants, does not practice the medical profession. The choice of the most suitable surgical intervention and technique is necessarily the responsibility of the holy professional. Each surgeon will have to evaluate the appropriateness of the implant technique he intends to carry out in the light of his own preparation, experience and clinical evaluation of each individual patient.
Your orthopedic surgeon is responsible for all recommendations and decisions about your medical care if you and your surgeon decide that joint replacement is appropriate for you. The following information also does not provide a complete or full discussion of the specifics of joint replacement surgery; the prosthesis that may be used; your care before, during, and after surgery; or the potential complications associated with surgery and your particular condition. Depending upon your particular condition, some of the general information provided may not be applicable to you. You will need to discuss the specifics of your case with your surgeon. LimaCorporate does not guarantee any specific results, recovery or rehabilitation.
WARNING: Please remember the information on this document is for educational purposes only and should not be used to make a decision on a condition or a procedure. All decisions should be made in conjunction with your surgeon and your primary care provider.
All rights to the video content are reserved in accordance with applicable law. Reproduction, publication and distribution by third parties are expressly prohibited without authorization.